The ever lasting question, Is it lymphoma?
HPI:
40-year-old man was referred to ED for abnormal MRI. 2 weeks prior to admission patient developed acute onset dysarthria with marked slurred speech. Patient presented to a local ED, CT head was negative and was diagnosed with tonsillitis and discharged home.
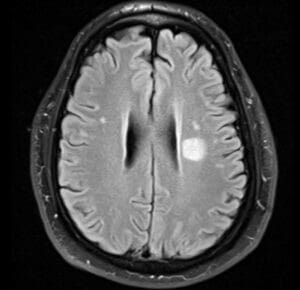
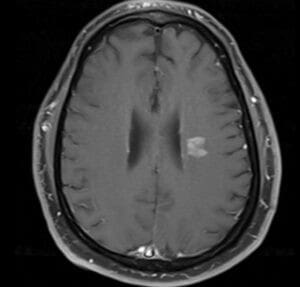
When symptoms persisted patient presented to his PCP, MRI was ordered and when MRI did show corona radiate enhancing lesion shown above, he was referred to ED again for further workup.
Examination:
Neurology was consulted, patient has no other symptoms than dysarthria. Exam with only slurred speech and right extensor planter response. No prior episodes of loss of vision or other focal neurological deficits.
Workup:
MRI: 1.5 cm corona radiata lesion on FLAIR image that enhance with contrast, no diffusion restriction. Multiple subcorictal and juxtacortical FLAIR hyper intense lesions but non-enhancing.
MRI reported as either subcortical infarction versus demyelinating disease versus lymphoma.
Other routine labs including CBC and BMP were all unremarkable
The first question is: WHICH ONE?
Workup started with screening for demyelinating disease and ischemic disease.
- MRI cervical and thoracic spine were negative for any FLAIR lesions.
- CSF with normal cell count, protein and glucose. OCB and IgG synthesis are pending
- CTA and TTE were negative
- The only vascular risk factor is diabetes, no prior coronary artery disease, kidney disease or retinopathy.
- No history of prior focal neurological deficits.
The second question: HOW SHOULD WE TREAT?
- The presence of multiple juxtaxortical lesions on MRI, decision was to go with a trial of pulse steroids for possible multiple sclerosis. Also, if it is ischemia, steroids will not hurt.
- Patient had marked improvement in his symptoms and dysarthria markedly improved.
WE MISSED IT!
- Radiology called for an addendum to the CTA report. Patient has enlarged tonsils and cervical lymphadenopathy !!
- We completely missed it..
- Biopsy did reveal lymphoma
- The location of lymphoma being peri-ventricular and subcortical is where most brain diseases are usually seen. It is a location where demyelinating disease, ischemic disease, infection and tumors may occur.
- Lymphoma can have different sizes and shapes, it can be small rounded/oval similar to demyelinating lesions or large with irregular enhancement mimicking infections and other tumors.
- Lymphoma can present in any age, in completely healthy patients. Even when it presents in immunocompromised patients, infection and other tumors are still on the differential.
- There is no single test that is sensitive and specific enough too diagnose lymphoma easily.
What are the main differentials?
- Demyelinating disease: in case of small contrast enhancing peri-ventricular lesion ? MS
- Subacute infarction: in case of small subcortical or corona radiate lesion, not restricting diffusion but enhances
- Infection: in case of irregular enhancement or ring enhancement
- Other tumors: if large with mass effect and irregular contrast enhancement
1- Get CBC, test for HIV and order MRI cervical and thoracic spine if it mimics demyelinating lesions or if patient has radicular/spinal symptoms.
2- Get CSF for EBV PCR, cytology flow cytometry, lactate dehydrogenase iso-enzyme 5, B-microglobulin, IgH rearrangements, proteomics and microo-RNA analysis.
3- CT chest, abdomen, pelvis and testicular ultrasound to screen for other lesions that can be biopsied.
-> If CSF cytology was positive then you have a diagnosis
-> If CT chest, abdomen, pelvis or testticular US showed another lesion -> go for biopsy
-> If all the workup is negative -> repeat CSF flow cytometry
-> If repeat flow cytometry is negative -> proceed with brain biopsy
Definitive tests:
- CSF Cytology: low sensitivity (30%) but highly specific (100%)
- Vitreous or retinal biopsy: moderate sensitivity but highly specific (100%)
- Brain biopsy: moderate to high sensitivity and high specificity (100%)
Highly suspicious:
- CSF flow cytometry: low sensitivity (70%) - moderate specificity
- Clonal IgH arrangement: low sensitivity (60%) - moderate specificity (85%)
- Elevated CSF anti-thrombin III: low sensitivity (76%) - high specificity (98%)
- RNA microanalysis: high sensitivity (96%) - high specificity (98%)
Suspicious:
- Increased CSF LD5: moderate (93%) - low specificity
- Increased B2 microglobulin: low sensitivity (70%) and specificity (75%)