Her Eyes Were The Clue!
A case that shows how subtle exam findings are pertinent to diagnoses and shouldn't be looked over
Reason for the consult: Altered mental status
Story: 63-year-old right-handed woman with history of migraine and anxiety who developed severe persistent nausea 4 months ago that was attributed to esophageal stenosis and duodenal ulcer. Nausea resolved after few weeks. Again 3 weeks ago developed severe nausea that patient didn't eat except few bites throughout the past couple weeks. Over the past 5 days, patient started to get confused, makes up stories and sometimes hallucinates seeing people in her room. No auditory hallucinations. In the same time over the past 5 days patient hasn't been able to stand or walk, feels wobbly. Patient doesn't some, drinks alcohol only one glass daily.
Pertinent examination:
- Mental status: awake, alert, oriented to place not time - couldn't name current president, able to perform serial 7s, confabulates when asked what she did today.
- Speech: normal
- Cranial nerves: horizontal ophthalmoplegia with horizontal gaze evoked nystagmus
- Motor exam:
- 5/5 in all extremities with intact reflexes and flexor plantars
- Sensory exam:
- Normal
- Coordination: mild ataxia in finger to nose bilateral
What is your first differential diagnosis so far?
Confusion without focal weakness, numbness, aphasia or field cuts has a lot of differentials. First thing comes to mind is metabolic encephalopathy that can be caused by tons of disorders. We usually start with basic workup (CT head, CBC, electrolytes, renal and liver functions, ammonia, TSH), we may add MRI, EEG or LP in certain cases of if initial workup is negative.
However, it wasn't only confusion that she had. She did have confabulation, horizontal ophthalmoplegia with gaze evoked nystagmus (GEN) which are characteristic of Wernicke's encephalopathy.
GEN is unique to cerebellum and brainstem lesions. Horizontal ophthalmoplegia is most common eye manifestation in Wernicke's encephalopathy patients. Eye manifestations usually progress from nystagmus to complete ophthalmoplegia in the following order:
- Nonsustained GEN
- Sustained GEN without gaze holding deficit
- GEN with Gaze holding deficit
- Bilateral abducent palsy
- Complete ophthalmoplegia
What is other differentials?
Miller Fischer variant although our patient had preserved reflexes, also wouldn't explain disorientation and confabulation. Hypophosphatemia can cause weakness and ophthalmoplegia but no limb weakness in our case. Central pontine myelinolysis but patient didn't have any risk factor. Botulism wouldn't explain altered mentation, also her pupils were intact.
What is next step?
Actually horizontal ophthalmoplegia was a striking feature on exam, along with the fact of severe malnutrition both made WE the working diagnosis. I first ordered blood thiamine level along with B2, B3, B6 and folate. Started thiamine replacement at 500 mg tid IV for 3 days then 250 mg bid IV for 5 days then 100 mg bid PO.
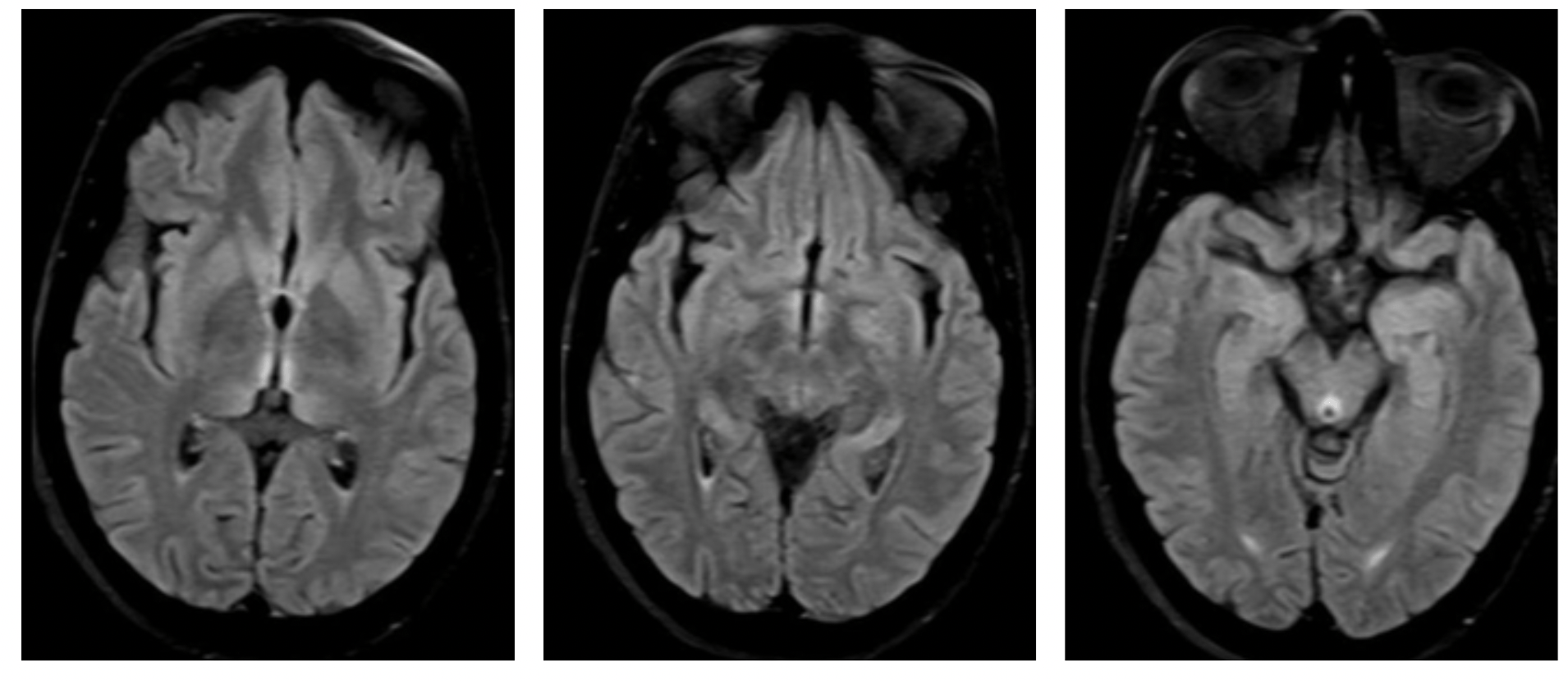
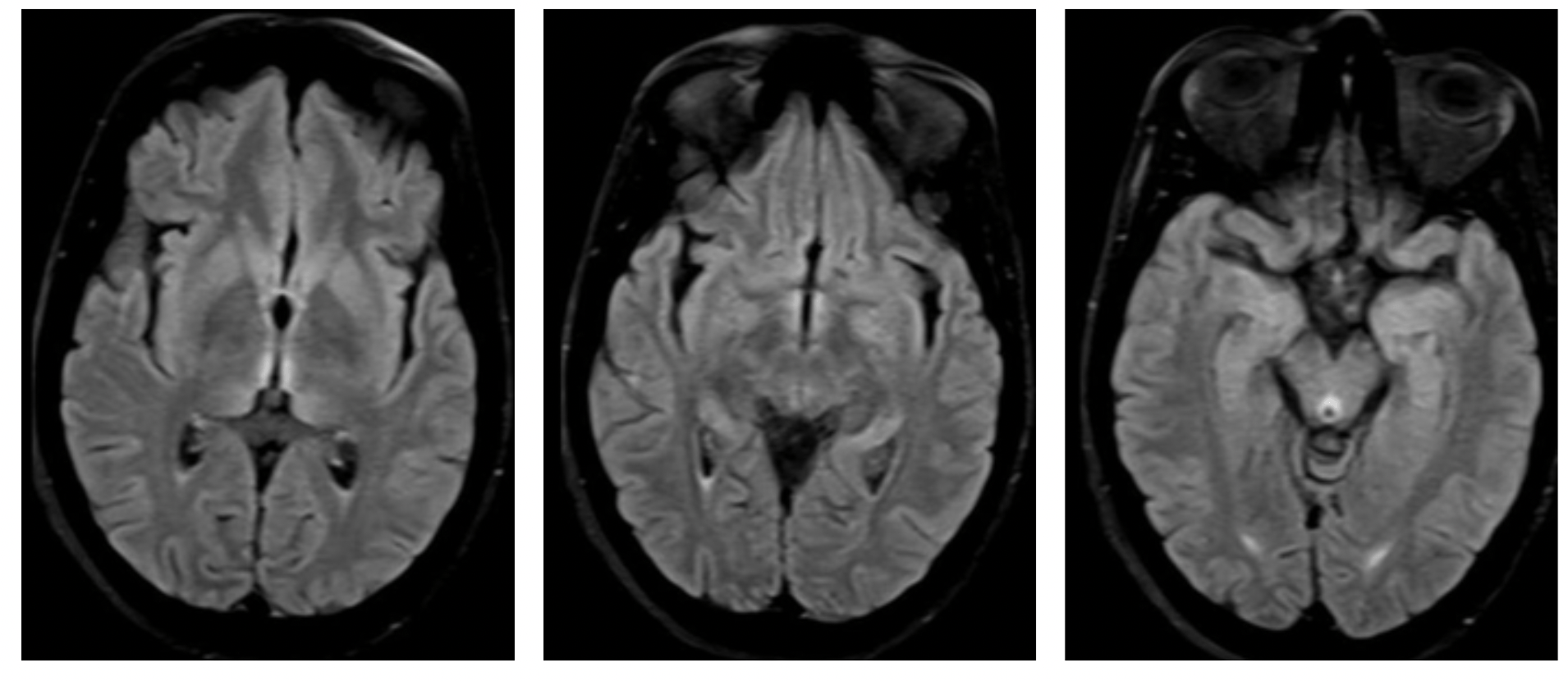
- MRI brain with contrast did show signs of WE, signal hyperintensity in: Bilateral medial thalami, maxillary bodies and peri-aquiductal gray matter.
What happened next?
- Next morning ophthalmoplegia had resolved, patient was oriented, still mild confabulation but generally improving.
Bottom line: Pay attention to every small detail in exam, everything has a meaning