Quick Facts:
- The optic nerve head is formed from a coalescence of 1 million axons from the retinal ganglion cells.
- The optic nerve is divided into the intraocular, intraorbital, intracanicular, and intracranial
- An altitudinal visual field defect is suggestive of ischemic optic neuropathy but may also be seen in idiopathic optic neuritis.
- Ischemic optic neuropathy is the result of posterior ciliary artery occlusion.
- 90% of ischemic optic neuropathy are nonarteritic and related to a congenitally small optic cup and 10% may have underlying giant cell arteritis.
- more
- 80% of patients with optic neuritis will have signal intensity abnormality within the optic nerve in STIR sequences with fat-suppressed views
- In the Optic Neuritis Treatment Trial (ONTT), 59% of patients had cerebral white matter lesions
- 56% of optic neuritis convert to MS in 10 years if MRI is positive and only 22% if MRI is negative
- The fibers of the optic tract synapse in: the primary visual pathway synapses in the LGB, the pupillomotor pathway synapses in the pretectum, and the subcortical visual pathway synapses in the superior colliculus
- Oculomotor complex is located in the dorsal midbrain, anterior to the cerebral aqueduct.
- The central caudal nucleus innervates both levator muscles
- The superior rectus receives information from the contralateral superior rectus subnuclei, but the rest of the innervation of the third nerve is ipsilateral.
- As the oculomotor nerve enters the orbit, it separates into the superior and inferior divisions. The superior division innervates the levator palpebrae and superior rectus, whereas the inferior division innervates the papillary sphincter, medial and inferior recti, and the inferior oblique.
- A lesion of the third nerve nucleus is exceedingly rare but will result in an ipsilateral third nerve palsy with contralateral superior rectus weakness and bilateral partial ptosis
- Trochlear nerve floats freely in the cavernous sinus lateral to the internal carotid artery, as opposed to the third and fourth nerves, which are in the lateral wall of the sinus.
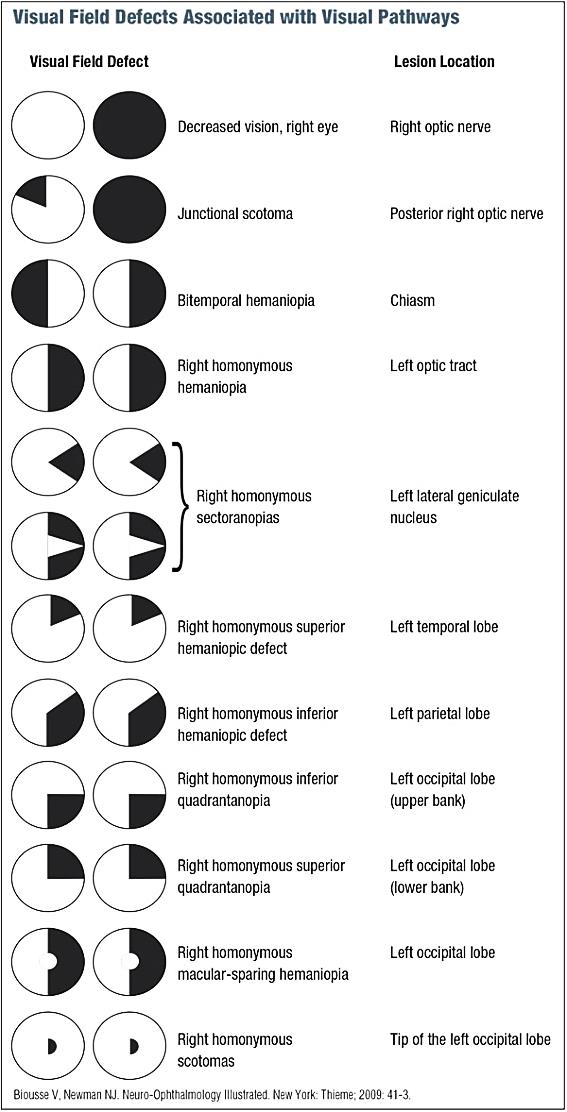
| Field Defect or Syndrome | Localization |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Syndrome | Localization | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Motility Disturbance | Localization/Etiology |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Abnormality | Description | Causes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|